Table of Contents
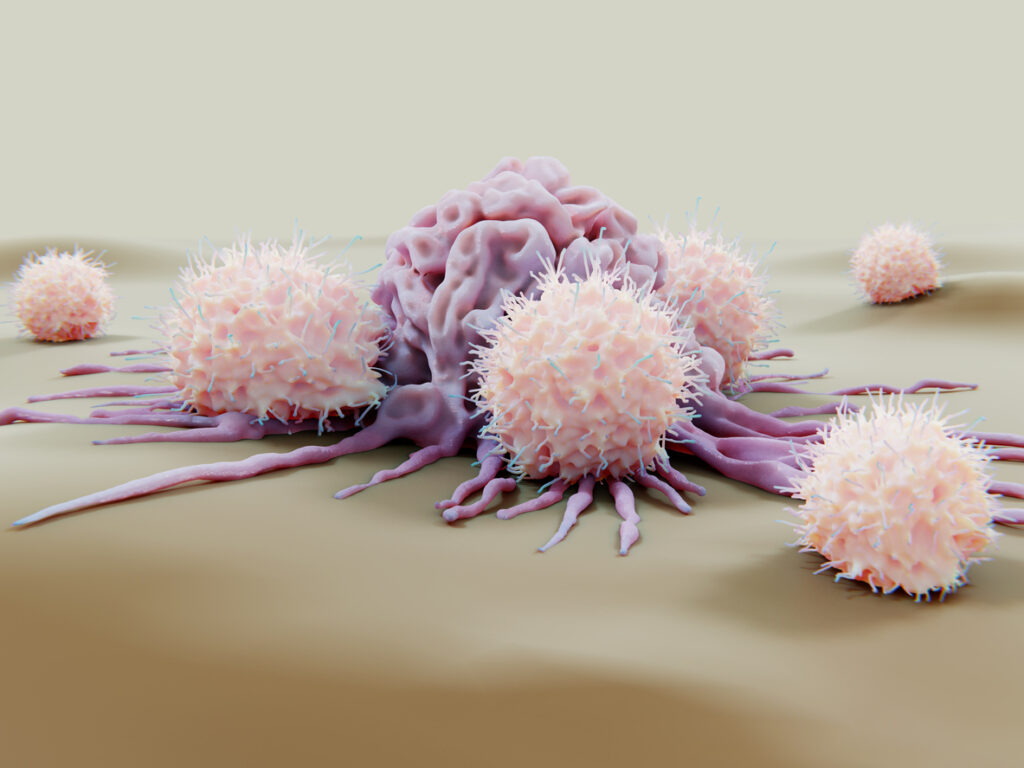
ToggleImmunotherapy harnesses the power of the human immune system to target and eliminate cancer cells, providing a promising approach in the field of cancer treatment. Natural killer (NK) cells, a kind of white blood cell, play a critical role in immune surveillance against tumors and infected cells. These cells have gained significant attention in immunotherapy due to their ability to directly kill cancer cells without prior sensitization.
To enhance the effectiveness of NK cells in cancer treatment, researchers have developed various protocols for expanding NK cells ex vivo, increasing their numbers, and allowing for activation before being introduced into the patient’s body.
Why Is NK Cell Expansion Necessary?
While NK cells are naturally present in our bodies, their numbers and activity may not be sufficient to overcome the challenges posed by cancer. Tumors often employ immune evasion strategies to suppress the function of NK cells, rendering them less effective in eradicating cancer cells.
Additionally, the nutrient and oxygen-depleted tumor microenvironment can further inhibit NK cell activity. Therefore, expanding NK cells ex vivo provides a means to overcome these limitations and strengthen the immune response against cancer.
NK Cell Expansion in CAR-NK Therapy
NK cell expansion is not only crucial for augmenting the natural anti-tumor immune response but also for advancing cutting-edge therapies like chimeric antigen receptor (CAR)-NK cells. CAR-NK cells are genetically engineered NK cells that express CARs on their surface, enabling them to specifically target cancer cells based on the expression of tumor-associated antigens.
The expansion of NK cells ex vivo allows scientists to genetically modify and grow these cells in large quantities, enhancing their tumor recognition and killing capabilities. In this way, researchers can create a potent and targeted cellular therapy that holds immense promise in the field of cancer immunotherapy.
Types of NK Cell Expansion
There are two primary approaches to NK cell expansion: in vivo and ex vivo. In vivo expansion involves administering cytokines, such as interleukin-2 (IL-2), or other immune-stimulating factors to the patient, enhancing endogenous NK cell proliferation. Although this approach has shown some success, it is often limited by the potential for systemic side effects and difficulties in achieving sufficient expansion levels.
Ex Vivo NK Cell Expansion Protocols
Ex vivo NK cell expansion involves isolating NK cells from a patient or donor and culturing them in a controlled laboratory environment. This approach offers several advantages, including optimizing expansion conditions, selecting desirable NK cell subsets, and activating the cells for improved cytotoxicity.
Feeder Cell-Based Protocols
Feeder cells—such as irradiated peripheral blood mononuclear cells (PBMCs), Epstein-Barr virus-transformed lymphoblastoid cell lines (EBV-LCLs), or K-562 cells—can be used to support NK cell culture expansion. Feeder cells provide essential growth factors and adhesion molecules that promote NK cell proliferation, but this method requires careful monitoring to avoid contamination and potential immune reactions.
K-562 cells, a human chronic myelogenous leukemia cell line, have become popular as feeder cells in NK cell expansion protocols. These cells cannot inhibit NK cell function and express ligands that activate NK cells through various receptors. K-562 cells can be modified to express membrane-bound cytokines, such as IL-15, further enhancing NK cell expansion and activation.
However, feeder cells can introduce complexities and potential concerns in NK cell expansion protocols. K-562 cells, while often used as feeder cells in NK cell expansion protocols, can exhibit variable behavior and may not reliably support optimal NK cell expansion.
Additionally, using K-562 cells as feeder cells requires meticulous monitoring to avoid contamination that may cause severe immune reactions in the patient. Feeder cells, including K-562 cells, may express certain molecules or ligands that can interfere with NK cell function or induce unintended immune responses. They also present a risk of introduction of an improperly irradiated cell line to a patient and evolution of a new cancer in vivo.
Cytokine-Based NK Expansion: An Alternative to K-562 Feeder Cells
Cytokine-based expansion is an ex vivo NK cell expansion protocol that offers several advantages over feeder cell-based expansion. Cytokine-only protocols avoid the variability of feeder cells and provide greater control over the expansion process, optimizing expansion conditions and generating a more homogeneous population of NK cells. This approach enables researchers to fine-tune their expansion parameters, such as culture duration and IL-2, IL-15, and IL-18 concentrations in the NK cell expansion media to achieve the desired NK cell phenotype and functionality.
Cytokine-based protocols also enhance simplicity and safety. By relying solely on cytokines, the approach offers a safer, more standardized method for NK cell expansion. Cytokine-based expansion eliminates the risk of contamination and proliferation of malignant cells, allowing for a more focused and controlled expansion of NK cells without risking potential side effects related to feeder cells.
The main disadvantage of cytokine-only approaches tends to be a slower and weaker initial NK cell activation, resulting in longer culturing times compared to feeder-cell approaches. However, these disadvantages are greatly reduced with the strategic inclusion of activation molecules, such as anti-NKp46 and anti-CD2 monoclonal antibodies.
CAR-NK Therapy Protocols
Expanding NK cells for CAR-NK cell therapy follows similar principles to traditional NK cell culture protocols, with the added step of CAR introduction via gene editing technologies. After the NK cells are isolated and expanded, they are genetically modified to express CARs that are designed to recognize specific antigens on cancer cells. This modification empowers CAR-NK cells to recognize and eliminate tumor cells more effectively. Subsequently, the expanded CAR-NK cells are validated and characterized before being used for therapeutic purposes.
The expansion of NK cells for CAR-NK cell therapy opens up exciting possibilities for precision cancer treatment. Due to their innate recognition mechanisms, CAR-NK cells offer several advantages over other cellular therapies, including reduced risk of graft-versus-host disease (GVHD). Unlike with CAR-T therapy, the NK cell donor does not have to be the patient, creating the potential for off-the-shelf use. Furthermore, the combination of NK cells’ innate cytotoxicity with the targeted antigen specificity of CARs creates a potent therapy that can overcome the challenges posed by tumor heterogeneity and immune evasion mechanisms.
Nanotein’s NanoSpark™ NK Cell Expansion Protocols
While feeder cells like K-562 cells have been widely used in NK cell expansion protocols in the past, cytokine-based expansion offers significant advantages. By eliminating the use of feeder cells, it provides enhanced control, simplicity, and safety in the expansion process while avoiding potential complications and side effects associated with feeder cells. As the field of immunotherapy continues advancing, cytokine-based expansion is emerging as a promising alternative, promoting the development of homogeneous and functional NK and CAR-NK cell populations for effective cancer treatment.
Reflecting these advancements, Nanotein developed an innovative new feeder-free NK cell expansion solution: NanoSpark™️️️️ GROW-NK Soluble Activator. This approach has all the high performance and protein-based benefits of our NanoSparkTM platform technology while fully compatible with several cytokine-combinations, including IL-2 and IL-15 cytokine-based NK cell expansion protocols ex vivo.
Contact our team to learn more about the benefits of feeder-free NK cell expansion with NanoSpark™️️️️ GROW-NK Soluble Activator.