Table of Contents
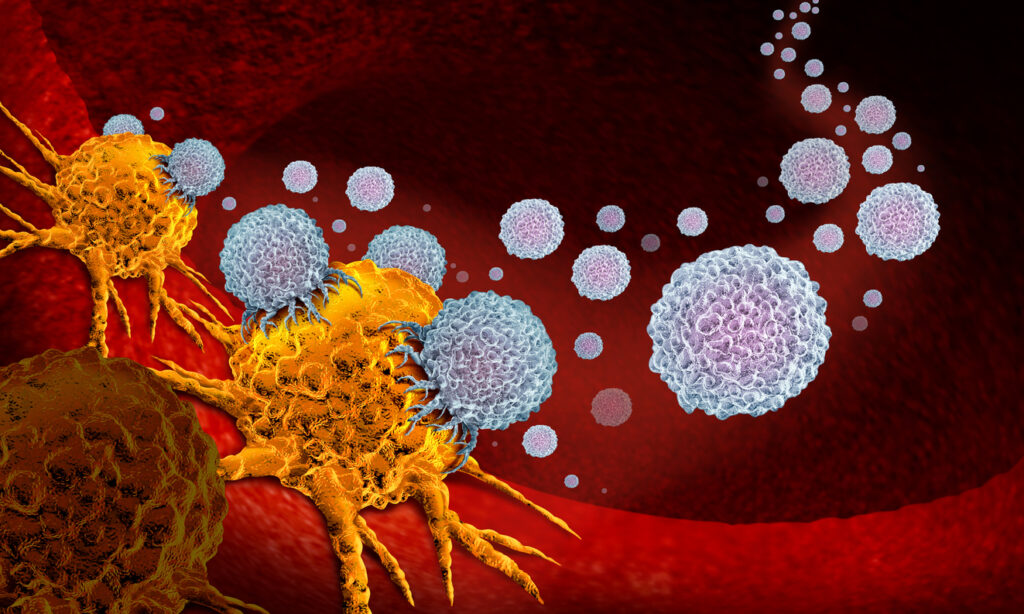
ToggleCAR-T cells, derived from a patient’s T cells, are genetically modified immune cells that hold immense potential in targeting and eliminating cancer cells.
What Are CAR-T Cells?
CAR-T cells—or chimeric antigen receptor T cells—are a type of T cell that have been genetically modified to enhance their ability to target and destroy cancer cells. Researchers derive CAR-T cells from a patient’s blood collected during leukapheresis at a medical clinic. The clinic then ships the concentrated white blood cells to the laboratory where scientists isolate T cells from the rest of the leukocytes.
In the lab, the T cells are genetically engineered to express a chimeric antigen receptor (CAR) on their surface. This allows the T cell to be activated through binding of a selected target on cancer cells, in vivo, without binding to an antigen-major histocompatibility complex (MHC) of an antigen-presenting cell (APC). In this way, CAR-T cells bypass many of the immune system’s typical activation mechanisms by directly recognizing cancer antigens and neutralizing the target cells they have been engineered for.
Once the patient’s T cells have been successfully modified, they are expanded in the laboratory in vitro to generate a large population of CAR-T cells. After undergoing rigorous quality checks, the CAR-T cells are infused back into the patient’s bloodstream, where they can circulate and target cancer cells throughout the body.
CAR-T Cell Structure
CAR-T cells retain most of the original T cell’s functional structure but with the critical addition of genes that will allow the cell to transcribe and express the CAR protein specifically designed to identify the patient’s cancer type.
The genes to program CAR expression are pulled from several different aspects of immunological function. They are recombined to transcribe a new membrane protein complex, lending to the “chimeric” nature of chimeric antigen receptor T cells.
An Introduction to CAR Proteins
CAR protein genomic constructs are integrated into T cells while activated in culture via viral vector transduction or transfection methods. The engineered receptor combines components from T cell and antibody receptors, resulting in a hybrid structure.
The CAR protein itself consists of three distinct regions:
- Ectodomain: This is the extracellular portion of the CAR that recognizes and binds antigens. The ectodomain contains an antigen recognition region and a spacer with a hinge domain that connects the ectodomain to the transmembrane domain. The antigen recognition domain comprises strategically selected single-chain fragment variants (scFv) of immunoglobulins (antibodies) that determine antigen recognition.
- Transmembrane domain: This portion of the CAR consists of a hydrophobic alpha helix that spans the membrane of the CAR-T cell—connecting the ectodomain to the endodomain—and directly affects the stability of the receptor. Studies show that the ectodomain hinge region and transmembrane domain also play a role in cytokine release.
- Endodomain: This intracellular domain contains functional signaling domains, such as CD3ζ, responsible for activating the CAR-T cell upon antigen binding. Additional costimulatory domains, such as CD28 or 4-1BB, are also included to provide further activation and enhance the persistence and efficacy of the CAR-T cells.
CAR-T Cells Can Target Specific Cells
The scFv design of the ectodomain’s antigen recognition region most directly determines the specific antigen target of a CAR-T cell. The domain can be customized to target different antigens, enabling CAR-T cells to be created for specific types of cancer.
The Food and Drug Administration (FDA) currently approves CAR-T therapies to target CD19 (a receptor found on the surface of most B cells that determines growth and development activity; often expressed by leukemia, lymphoma, and myeloma cells) and BCMA (an important signaling receptor found on mature B cells; often expressed by lymphoma and myeloma cells).
The current FDA-approved therapies are based on the second generation of CAR-T cell design that includes the addition of the CD28 or 4-1BB costimulatory domains. While showing great promise, these therapies still have the potential for severe life-threatening toxicities (such as cytokine release syndrome), modest anti-tumor activity, and antigen escape.
Several generations of CAR-T cells are now being iterated on for more reliable activation and to better target and neutralize cancer cells in vivo. However, these new generations of CAR-T technology still rely on finding efficient, non-toxic CAR-T cell activation and expansion ex vivo methods.
Nanotein Specializes in CAR-T Cell Expansion
Many current ex vivo activation and expansion techniques introduce clinical risks to the process by using synthetic ingredients and magnetic beads that may contaminate the CAR-T therapy product if not painstakingly removed from the expanded culture.
To address this, Nanotein Technologies developed a novel protein-based CAR-T technology in a soluble format that requires less time, fewer T cells, and no magnetic components or synthetic contaminants. Nanotein’sNanoSpark™ STEM-T Soluble T-Cell Activator focuses on TSCMs CAR-T expansion, generating large quantities of clinically potent CAR-T cells in a less differentiated state for increased self-renewal ex vivo and clinical safety during treatment.
Contact our team today to learn more.