Table of Contents
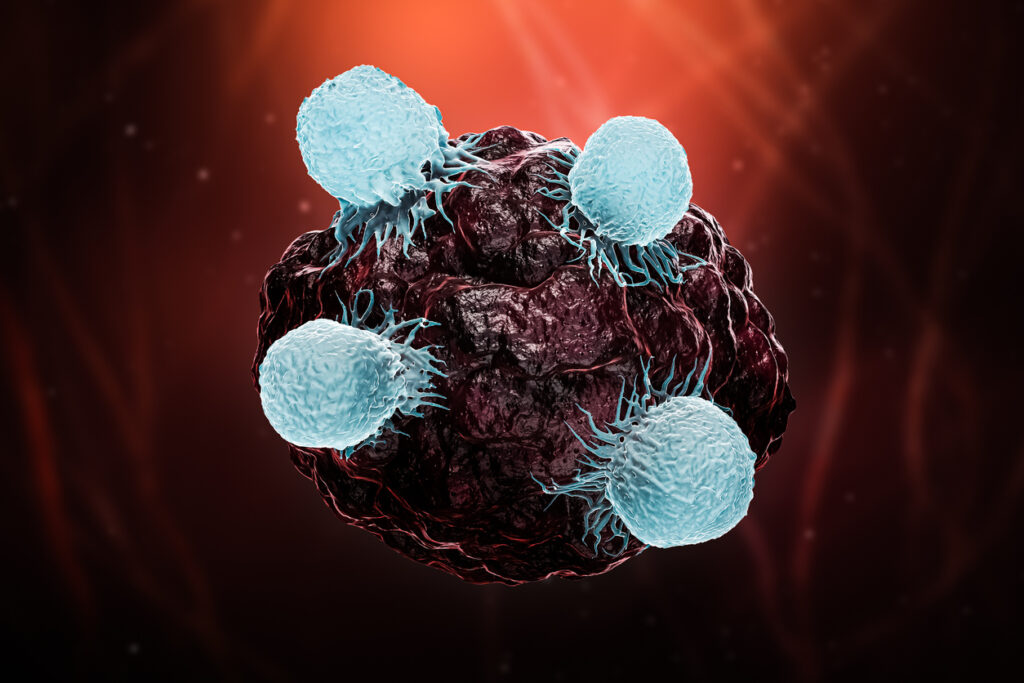
ToggleCD8+ T cells, also known as cytotoxic T cells or “killer T cells”, play a crucial role in the human immune system’s defense against infections and cancer. Once activated, these specialized white blood cells recognize and eliminate virus-infected or abnormal cells by releasing toxic substances that induce cell death. CD8+ T cells differentiate along a continuum of subset cell types vital in maintaining overall health and preventing disease spread.
What Is a CD8+ T Cell?
CD8+ T cells are a subset of T lymphocytes that express the CD8 protein on their cell surface. They are generated in the thymus from progenitors originating from bone marrow stem cells but lack the coreceptors necessary to be considered mature T cells.
During this process, called thymic selection or thymopoiesis, T cells undergo a series of positive and negative selection steps that enable them to recognize and respond to the presentation of antigens. This includes gaining functional coreceptors like CD8 and CD4.
Specifically, CD8+ T cells are characterized by the presence of the dimeric CD8 coreceptor, which, in conjunction with T cell receptors (TCRs), interacts with major histocompatibility complex class I (MHC I) molecules on the surface of antigen-presenting cells (APCs). This coreceptor allows CD8+ T cells to recognize antigens presented by MHC I molecules. These antigens are typically derived from intracellular pathogens or abnormal cellular components.
CD8+ T Cell Function
CD8+ T cells are vital to many aspects of the immune system. Their main functions include cell-mediated cytotoxicity, defense against viral and intracellular pathogens, tumor surveillance, memory response, and regulatory maintenance. However, CD8+ T cells primarily neutralize or “kill” diseased cells during the initial stages of infection or tumor response.
How Do Cytotoxic T Cells Kill?
Cytotoxic T cells function as killer effector cells through three major mechanisms:
- Cytotoxic granules: CD8+ T cells produce and release two families of protein granules—perforin and granzymes—that have direct cytotoxic effects on diseased cells. Perforin punctures a pore in the target cell’s membrane, similar to the function of complement, a plasma protein family that also opsonizes pathogens. This pore allows granzymes, a type of serine protease, to enter the target cell and begin cleaving proteins inside of the cell. This shuts down cellular protein production and eventually results in target cell apoptosis. Natural killer (NK) cells also release these cytotoxic granules.
- Fas/FasL interactions: Activated CD8+ T cells destroy other cells by expressing the FasL protein on their surface. FasL binds to Fas, a surface receptor on the target cell. Binding causes the target cell’s Fas molecules to trimerize, pulling together signaling molecules that activate the caspase cascade. This cascade leads to apoptosis of the target cell. Interestingly, CD8+ T cells express both FasL and Fas and other “death factors” which can result in suicide or fratricide (when T cells eliminate each other) of the cells. This is an important regulatory function known as activation-induced cell death (AICD) that encourages T cell population contraction at the end of an immune response.
- Cytokine secretion: CD8+ T cells also indirectly kill malignant or infected cells via the secretion of cytokines—like tumor necrosis factor alpha (TNF-α) and interferon-gamma (IFN-γ). IFN-γ enhances the presentation of antigens and inhibits viral replication. TNF-α is a pleiotropic effector, meaning it has significant roles in both pro-inflammatory and anti-inflammatory immune mechanisms. As a pro-inflammatory signaling molecule, TNF-α induces dendritic cell activation, naive and memory T cell differentiation, sustains T cell survival, and encourages other anti-tumor activity. TNF-α also promotes anti-inflammatory responses, such as apoptosis of highly activated effector T cells and mediating regulatory T cell (Treg) activity.
CD8+ T Cell Activation
Naive CD8+ T cells are activated by recognizing antigens displayed on the MHC Class I complex of specific antigen-presenting cells (APCs), such as dendritic cells. The binding of the CD8+ T cell’s TCRs to the antigen-MHC complex typically requires costimulatory signals to fully activate and ensure the T cell response is appropriately regulated.
CD28 is the primary coreceptor in this process and the standard activation mediator both in vivo and when stimulating T cell culture for activation ex vivo. This binding then initiates signal transduction within the naive CD8+ T cell, activating various intracellular signaling pathways that in turn, result in activation, differentiation, and clonal expansion.
Additional cytokines and molecules are critical for enhancing and regulating an immune response’s activation and expansion phase. The presence of certain related interleukin (IL) proteins that are produced by white blood cells, such as IL-2 and IL-7/ IL-15, are especially important when T cells are manufactured for adoptive immunotherapy applications, as growing APCs in the culture media to present antigens is not practical. Researchers can even tailor cytokine selection to increase activation and expansion of certain T cell subsets.
CD8+ T Cell Exhaustion
Exhaustion is a state of immune cell dysfunction that occurs in chronic viral infections, cancer, and other persistent antigenic stimulation scenarios. Exhausted CD8+ T cells gradually lose the effector functions that allow them to eliminate infected or cancerous cells effectively. This includes decreased production of cytotoxic granules and cytokines, upregulation of inhibitory receptors, and transcriptional changes that result in altered gene expression patterns.
Many immunotherapies combat T cell exhaustion by attempting to reinvigorate the cells directly with inhibitory receptor blockades or through the initial enrichment of certain T cell subset populations during ex vivo activation that are inherently less prone to exhaustion.
CD8+ T Cell Subsets
CD8+ T cells are divided into subsets based on their phenotype, functional properties, and expression of specific markers. Activated mature CD8+ T cells that eliminate infected or abnormal cells are generally referred to as cytotoxic effector T cells. However, memory CD8+ T cells and, more recently suggested, regulatory CD8+ T cells also have critical and often overlapping roles in the immune response process. The lines between these categories are unclear and—as with the maturation process of T cells in general—exist along a continuum.
Memory CD8+ T Cell
Memory CD8+ T cells persist after the initial immune response and provide long-term immunity against re-infection. They can quickly respond to a recurring infection, mount a quick and strong immune response, and help control the disease more effectively.
Some types, like effector memory CD8+ T cells (TEM), patrol the peripheral tissues and exhibit direct effector functions. They have a low proliferative capacity but provide rapid and localized immune responses. Other types of memory T cells, like central memory T cells (TCM), reside in the lymphoid tissues and do not actively exhibit effector functions. However, they have a high capacity for self-renewal and rapidly differentiate into effectors cells upon re-encountering the antigen.
Some even less differentiated memory cell types, such as stem cell memory T cells (TSCMs) are especially ideal for adoptive immunotherapy applications because of their capacity for proliferation and self-renewal.
Regulatory CD8+ T Cell
Regulatory CD8+ T cells, or CD8+ Tregs, are a subset of CD8+ T cells that exhibit immunosuppressive and regulatory functions. While CD4+ Tregs have been well-studied and characterized, the understanding of CD8+ Tregs is relatively more recent and still an area of ongoing research.
CD8+ regulatory T cells suppress the activity of other immune cells, including CD4+ T cells, CD8+ effector T cells, B cells, and antigen-presenting cells (APCs). Their suppressive activity helps to prevent excessive immune responses and maintain immune homeostasis. This modulation results from cell-to-cell surface molecule interaction and binding, cytokine secretion, and metabolic regulation.
However, the study of CD8+ Tregs is still evolving, and researchers continue to investigate their detailed mechanisms of action, functional properties, and potential therapeutic applications.
CD8+ Cells vs. Other Cell Types
CD8+ T cells collaborate with other immune cells, such as CD4+ helper T cells, B cells, NK cells, and APCs to orchestrate immune responses effectively. The effector attributes of CD8+ T cells mainly derive from the presence of the CD8 co-receptor and primary recognition of antigens presented on MHC Class I molecules that trigger cytotoxic mechanisms.
However, immune cell subsets are not definitive. Some T cells have both CD8 and CD4 T cell coreceptors, and the ratio of these receptors drives overall function and, therefore, classification.
Alternatively, NK cells have some overlapping cytotoxic effector functions as CD8+ T cells but they are a part of the innate immune system—not the adaptive immune system—and can recognize and kill target cells without prior antigen exposure. B cells are largely responsible for the humoral aspect of adaptive immunity, providing long-term memory protection and producing antibodies when differentiated into plasma cells.
Nanotein Expands CAR-T Cells for Cancer Immunotherapy
Given the importance of CD8+ T cell function throughout the immune response, scientists at Nanotein Technologies have developed products specifically tailored to activate and expand T cells for cancer immunotherapy and other therapeutic research applications.
Especially useful for CAR-T technology applications, NanoSpark™ STEM-T Soluble T Cell Activator efficiently enriches CD8+ T cells for ex vivo activation and expansion. The Nanospark STEM-T technology even specifically expands less differentiated CD8+ TSCMs cells to enhance proliferation, self-renewal, and resistance to exhaustion.
Contact us today to learn more.