Table of Contents
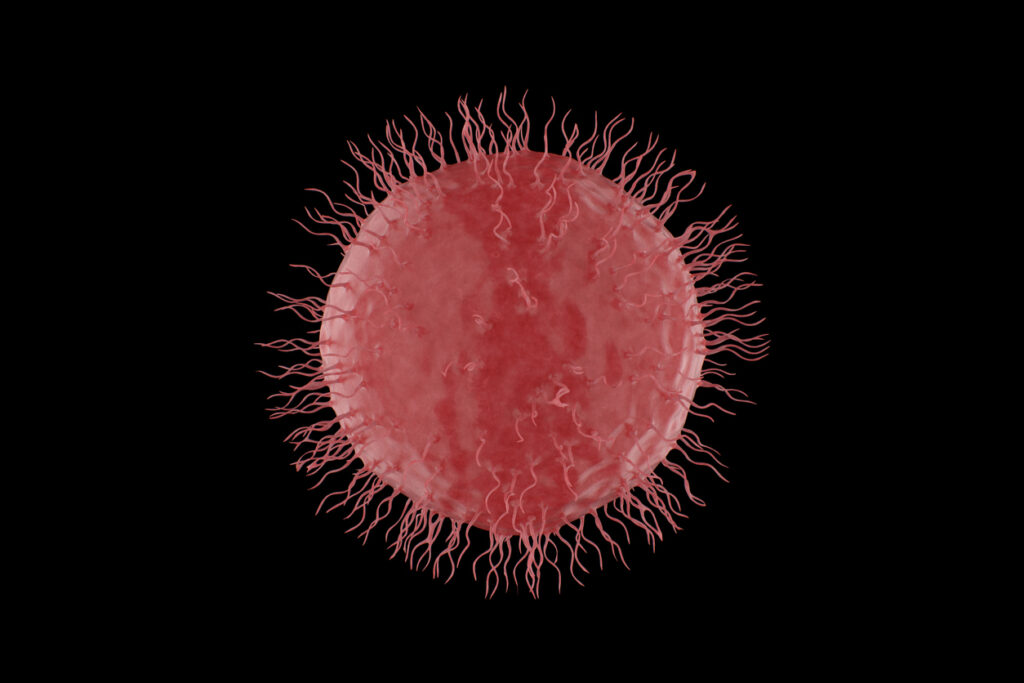
ToggleThe immune system is an intricate nexus of cells and molecules protecting the body against pathogens and diseases. Among the defenders of this intricate system, natural killer (NK) cells are crucial to activating and maintaining a healthy immune response.
What Are Natural Killer Cells?
NK cells are a specialized subset of lymphocytes that are a vital component of the innate immune system. They are present in various tissues, including the blood, liver, and lymph nodes. NK cells are characterized by their ability to recognize and eliminate infected or malignant cells without prior sensitization.
However, scientists have also demonstrated that NK cells readily adjust to their environment and form antigen-specific immunological memory. This unique ability also gives them a role in the adaptive immune system.
Origins of NK cells
Like other white blood cells, natural killer cells originate from hematopoietic bone marrow stem cells and undergo a series of coordinated maturation and differentiation processes. During development, NK cells acquire different phenotypes and functional capabilities, leading to the classification of distinct subsets. The two major types of NK cells are cytotoxic (CD56dim) and immunoregulatory (CD56bright) NK cells, each with unique functions in immune surveillance.
NK Cell Function
- Surveillance and early defense against infections: NK cells serve as a vital first line of defense against viral infections and other pathogens. Equipped with specialized CD16 receptors, CD56dim NK cells can identify virus-infected cells and initiate their elimination through direct cytotoxicity. This rapid response prevents viral replication and limits the spread of infection. NK cells also excel at recognizing and targeting cancerous cells, a process known as tumor surveillance.
- Modulation of the immune response: CD56bright NK cells interact with other immune cells to regulate immune responses. They engage in cross-talk with dendritic cells, macrophages, and T cells, influencing the outcome and intensity of immune reactions. By producing specific cytokines, such as interferon-gamma (IFNγ) and TNF-alpha (TNFα), NK cells shape the immune environment and help to facilitate appropriate immune reactions.
- Immunoregulation during pregnancy: NK cells are also critical in maternal-fetal immune tolerance during pregnancy. They interact with trophoblast cells in the placenta, ensuring a suitable immunological environment is established and maintained for a successful pregnancy. The delicate balance maintained by NK cells supports fetal growth and development while preventing rejection by the maternal immune system.
Mechanisms of Natural Killer Cell Activity
NK cells employ a range of cellular mechanisms to carry out their functions.
Recognition of Target Cells and NK Cell Activation
NK cell surfaces have several activating and inhibitory receptors. These receptors bind ligands of target cells and enable them to distinguish healthy cells from infected or cancerous cells. Activating receptors trigger NK cell responses, including:
- Natural cytotoxicity receptors (NCR) enable NK cells to bind and eliminate virus-infected cells and modulate the release of cytokines, such as IFNγ. NCR also has a role in eliminating bacterial infections and tumor growth recognition.
- CD16 facilitates antibody-dependent cell-mediated cytotoxicity (ADCC) coordinated by plasma cells’ release of antibodies. CD16 specifically binds immunoglobulin G (IgG) type antibodies, the most common antibody in human blood.
- Toll-like receptors (TLR) are the hallmark pattern recognition receptors (PRRs) of the innate immune system. TLRs recognize pathogen- and damage-associated molecular patterns on diseased cells. TLRs are continuously expressed on NK cells independent of activation status and thus are crucial to enabling NK activation by binding diseased cells and initiating the overall immune response.
Alternatively, inhibitory receptors prevent NK cells from attacking healthy cells. These receptors include killer-cell immunoglobulin-like receptors (KIRs) and the CD94/NKG2 heterodimer functional protein receptor pair. Both KIRs and CD94/NKG2 receptors recognize the major histocompatibility complex class I (MHC I) of regular cells, inhibiting NK killing.
Cytokines released by other immune cells, such as CD4+ T cells, and macrophages, including interleukin-2 (IL-2), IL-12, and IL-15, also significantly modulate NK cell activation. The balance of all of these activating and inhibitory mechanisms allows NK cells to selectively target aberrant cells while sparing healthy tissues and preventing autoimmune reactions.
Killing Mechanisms and Cytokine Production
Upon recognition and activation, NK cells release cytotoxic granules containing perforin and granzymes upon recognition and activation. Perforin creates pores in the target cell membrane, facilitating the entry of granzymes. These proteolytic enzymes induce apoptosis in the target cell. NK cells also induce cell death by directly engaging death receptors on the target cell surface. However, natural killer cells are non-phagocytic, meaning they do not ingest and eliminate cells like macrophages and dendritic cells do.
In addition to their cytotoxic activities, NK cells secrete a range of cytokines that influence the immune response. These cytokines can modulate the behavior of other immune cells, regulate inflammation, and enhance the immune system’s overall efficiency. The secretion of IFNγ activates macrophages that play a major role in the lysis and phagocytosis of diseased cells. In addition, NK cells release TNFα, which enhances and promotes NK cells to bind and eliminate tumor cells directly.
Role of Natural Killer Cells in Disease
NK Cells vs. T Cells
The immune system encompasses a wide array of specialized cells, each with its unique functions and characteristics. As discussed, natural killer cells are vital to initiating and maintaining the innate immune system when a pathogen is first encountered. However, in order to maintain a multifaceted and robust approach to immunity, many functions of the body’s immune cells overlap, despite being activated through different mechanisms.
T cells are a prime example. Both CD56dim NK cells and CD8+ T cells are lymphocytes that induce cell death, eliminating pathogens through the release of granzymes and other cytotoxic means. Similarly, CD56bright NK cells and CD4+ helper T cells both recruit and coordinate other immune cells through the use of cytokines.
The key difference between NK cells and T cells lies in the necessity for the presentation of target antigens by the MHC of antigen-presenting cells (APCs), which is also a core differentiator between the body’s innate and adaptive immune response. All T cells require the presentation of antigens by APCs to initiate activation, creating a highly specific immune response to that antigen. Whereas, NK cells act as an immediate defense mechanism without the need for prior antigen exposure or activation by MHC.
Furthermore, T cells undergo a far more complex process of maturation and selection in the thymus, where their receptors are shaped and their self-reactive cells are eliminated. In contrast, NK cells do not undergo such a restrictive selection process and are innately tolerant to the body’s cells due to their inhibitory receptor interactions.
Like NK cells, natural killer T cells (NKT) bridge the divide between the innate and adaptive immune system, sharing characteristics from both NK and T cells. They have the ability to produce cytokines rapidly, exert cytotoxicity, and regulate the immune response. However, NKT cells express T cell receptors and carry out related functions, placing them on the T cell side of the category divide.
NK Cell Dysfunction
Clinical researchers traditionally associated autoimmune disease with the malfunction of T cells and B cells in the adaptive immune response. However, altered NK cell activity has recently been implicated in various diseases, such as systemic lupus erythematosus, autoimmune liver disease, and type I diabetes.
Deficiencies or dysregulation of NK cells have also been found to lead to increased susceptibility to viral infections, such as HIV and hepatitis, as well as contribute to cancer progression and metastasis.
Therapeutic Potential and Applications
Natural killer cells are indispensable components of the immune system, exhibiting diverse functions that encompass surveillance against infections, immunoregulation, and immunotolerance during pregnancy. Through their intricate mechanisms of recognition, activation, and killing, NK cells contribute to maintaining immune homeostasis. As our understanding of NK cells continues to expand, so does the potential for therapeutic interventions aimed at harnessing the power of these remarkable cells.
NK cells’ unique capabilities have sparked interest in developing NK cell-based immunotherapies for the treatment of infectious diseases and cancer. Researchers are exploring strategies to enhance NK cell function and improve their efficacy in targeting and eliminating malignant cells.
Like in CAR-T cell therapy, chimeric antigen receptors (CARs) can be engineered to enhance the targeting of different tumor-specific antigens and establish novel activation pathways to bolster the overall immune response. CAR-NK therapies are even showing a significant reduction in cytokine release syndrome (CRS) compared to CAR-T immunotherapy, leading many in the field to believe that it could be a safer alternative to solely T cell-based therapies. In addition, NK cell therapies can be derived through allogeneic methods, taken from human donors other than the patient without causing immune rejection.
However, NK cells can be tricky to expand ex vivo, often requiring co-culturing with cancerous feeder cells in order to get NK cells to activate and proliferate, complicating the manufacture of bulk immunotherapies and leading to a downstream risk for patients. This area of study is still very new, and more in-depth studies and clinical trials must be conducted before CAR-NK becomes a viable option for commercial use.
Nanotein’s NanoSparkTM Activator Promotes NK Expansion Ex Vivo
Given the vast therapeutic potential of NK cells, Nanotein Technologies has developed a first-in-class NK cell soluble activator that does not require the co-culture of feeder cells to achieve expansion ex vivo.
The NanoSpark™ GROW-NK Soluble Activator builds on the innovative NanoSparkTM platform technology that already includes the NanoSpark™ STEM-T Soluble T Cell Activator for high-performance enrichment without the need for magnetic beads.
Contact our team today to learn how to integrate NanoSparkTM NK cell expansion into your workflow.