Table of Contents
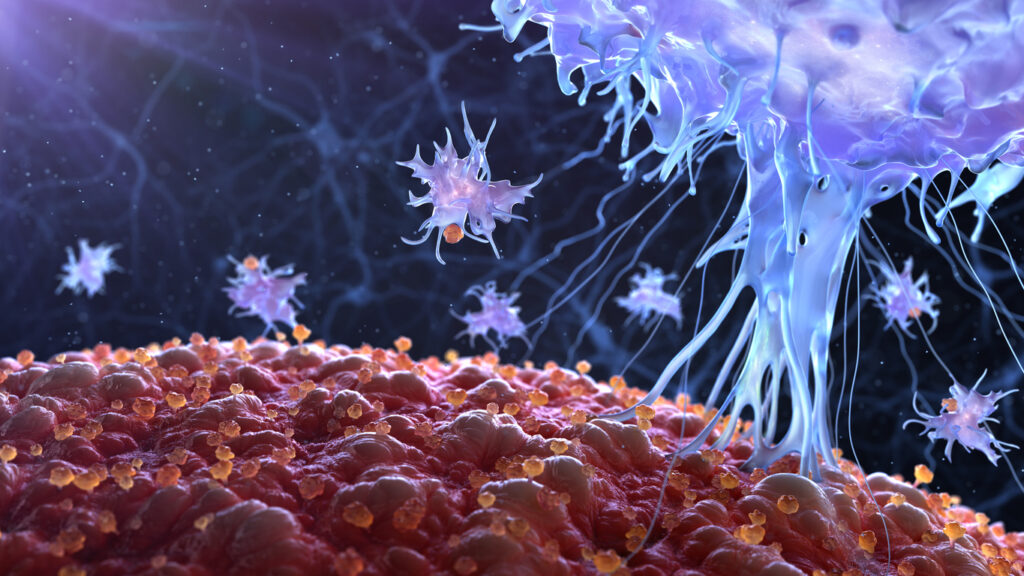
ToggleThe immune system of the human body is a complicated and integrated network of organs, specialized immune cells, and signaling pathways that work together to repel and neutralize disease-causing pathogens and toxins.
All immune system cells originate from blood stem cells produced in the bone marrow. Growth factor signaling molecules secreted by cells throughout the body determine how the maturation of these stem cells initially proceeds through their immune cell lineage.
Immune Response Mechanism
An immune reaction relies on both innate and adaptive cells in the immune system to work together to create a formidable and cohesive response to dangerous pathogens. Innate immunity is the body’s first line of defense. Its mechanisms include the physical and chemical barriers of epithelial cells, blood proteins that mediate inflammation, and immune cells that do not differentiate between unique pathogens. The immune system’s innate cells include dendritic cells, natural killer (NK) cells, and phagocytic neutrophils and macrophages.
In contrast, the adaptive immune system specializes in the recognition and destruction of a specific pathogen, toxin, cancer, or other foreign substance. Memory cells form that detect these antigens and induce a more vigorous response with repeated exposure. Whether new or remembered, an adaptive immune response ultimately leads to the production and binding of antibodies specific to a particular antigen. Once bound, the antigen is more easily recognized and neutralized by the immune system.
Immune Cell Types
Each immune cell type has a unique role in the overall immune response. A brief overview of major immune system cells and their interaction is described below, including what cells produce antibodies.
T Cells
T cells are a large family of the lymphoid immune cell lineage, maturing in the thymus, residing in the body’s lymphatic system tissues, and circulating in the blood. Newly matured T cells remain in a naive state until activated, triggering an adaptive immune response. T cells are distinguished from other lymphocytes by the presence of antigen-detecting T cell receptors (TCRs) on their cell surface.
Helper T cells (CD4+) and cytotoxic T cells (CD8+) activate when major histocompatibility complexes (MHC) on another cell present an antigen or specific peptide sequence to them. Following activation, helper T cells release small signaling molecules called cytokines which further direct and mediate the immune response via cytotoxic T cells, macrophages, and memory B cells.
Cytotoxic T cells are the primary effector cells of adaptive immunity and, once activated, can migrate through the walls of blood vessels and non-lymphoid tissues, including the blood-brain barrier. Once their antigen target is encountered, they may attack and destroy the cells displaying it directly or use cytokine signaling to recruit macrophages and natural killer (NK) cells to neutralize the invader or infection.
Memory T cells are also derived during the antigen presentation and T-cell activation process. Memory T cells live longer than other T cells and mitigate infection recurrence. Once reactivated by a previously encountered antigen, memory T -cells quickly proliferate and differentiate into many effector T cells.
Natural killer T cells (NKT), not to be confused with NK cells, are a bridge between the innate and adaptive immune systems. Unlike other T cells that recognize peptides and antigens presented by MHC, NKT cells recognize glycolipid antigens presented by CD1d on the surface of other antigen-presenting cells (APCs).
NKT cells express both TCRs, which are characteristic of adaptive immunity, and surface receptors of NK cells, which are part of the innate immune response. NKT cells influence tumor surveillance, autoimmune disease regulation, and maintenance of self-tolerance.
There are other members of the T cell family whose mechanisms of action have not been fully characterized. Notable among these are regulatory T cells that help shut down T-cell mediated immune responses toward the end of an immune reaction and suppress defective autoreactive T cells produced during the maturation process in the thymus. Both actions are critical to the maintenance of immunological tolerance.
B Cells
B cells are also a subset of the lymphoid immune cell lineage. Mature naïve B cells in the bone marrow become transitional B cells as they migrate to the spleen and lymph nodes. They activate by binding to antigens using B cell receptors (BCRs) on their membranes, often mediated by cytokines from helper T cells.
Once activated, B cells proliferate and differentiate into antibody-secreting effector cells called plasma cells. While T-cell independent activation is quicker, the antibodies produced tend to have lower affinity to the antigen and are not as functionally adaptable as those generated from T-cell mediated activation. Antibodies are highly specific immunoglobulin proteins that neutralize antigens by blocking infectivity, tagging for phagocytosis by macrophages, and inducing lysis directly or with the help of the complement system.
Memory B cells are created when B cells bind and take up antigens through receptor-mediated endocytosis. The antigen is degraded and presented as peptide pieces to T cells as one of several MHC expressing cells that can activate helper T-cell response. While memory B cells themselves do not produce antibodies, they are long-lived cells that may be driven to differentiate into antibody-producing plasma cells should a re-exposure occur.
Monocytes and Macrophages
Monocytes are large white blood cells of the myeloid immune cell lineage that circulate in the bloodstream. They are a part of the innate immune system, engulfing and digesting foreign substances and cellular debris in a process called phagocytosis.
Digested antigens may be presented to T cells via the MHC molecule to induce an adaptive immune response. Monocytes typically only circulate in the blood for a couple of days before migrating into tissues and becoming macrophages or some type of dendritic cells. Macrophages help tissues during wound healing through similar functions of phagocytosis and may reside in the tissue for months to years.
Dendritic Cells
Like monocytes and macrophages, dendritic cells are myeloid lineage APCs of the innate immune system. They process and present antigens to T cells and B cells via MHC molecules on their membranes. Dendritic cells are believed to be the only APC capable of activating naïve T cells.
Granulocytes
Granulocytes are effector white blood cells of the innate immune system that dominate the early response phase. This family of myeloid derived immune cells includes eosinophils, neutrophils, and basophils that release antimicrobial agents and enzymes toxic to pathogens and induce inflammation.
Some cells, such as neutrophils, also ingest microbes during the neutralization process. Mast cells are a particular type of granulocyte found in the body’s connective tissue that release histamine, mediating the removal of allergens from the body.
NK Cells
Natural killer cells are lymphoid derived immune cells that are primary effector cells of the innate immune system. They recognize infected or otherwise distressed cells in the body, such as tumor cells, and destroy them. While their function is analogous to cytotoxic T cells, they are considered lymphocyte-like and not true lymphocytes because they lack receptors to have fine target specificity.
Immune Cell Markers
All of these immune cells are primarily categorized and differentiated by the types of receptors, ligands, and other cell surface molecules found on their membranes. The vast variety of these identifying functional markers enables scientists to isolate groups of immune cells by type.
Unlike filtering or gradient centrifugation—which relies on the gross physical properties that often overlap with other cell types—cell marker isolation uses the unique binding relationship of marker molecules and their corresponding antibodies. Some common techniques include immune precipitation and immunomagnetic selection.
Related antibody binding techniques have also been used to sort lymphocytes via microfluidics and flow cytometry. These methods allow scientists to select the desired cell types and remove undesired ones, creating an enriched concentration of immune cells that can then be artificially activated and undergo expansion for downstream applications and medical therapies.
Applications of Immune Cells
The ability to isolate, activate, and initiate expansion of beneficial immune cells via their immune cell markers has greatly advanced the field of immunotherapy. However, rejection of foreign immune cells by the patient’s immune system remains one of the greatest challenges to cell-based immunotherapies for cancer and other immune modulated disease.
These therapies can cause potentially fatal side effects during treatment, including unchecked inflammation, hyperactivation of immune cells, and elevated levels of circulating cytokines. Fortunately, the latest immune cell marker mediated isolating techniques have enabled advantageous types of immune cells to be collected directly from a patient to reduce the likelihood of these side effects. NK cells and T cells are prime targets for this process because of their inherent ability to kill unwanted cells directly.
In one type of personalized cancer immunotherapy, a patient’s T cell isolates are genetically re-engineered to produce enhanced proteins on their surface called chimeric antigen receptors, or CARs. These CAR-containing T cells (CAR-T cells) bind more effectively to specific antigens on the surface of cancer cells, particularly effective in blood cancers (i.e. liquid tumors). Similarly engineered, CAR-NK cells have been shown to better survive the often harsh and toxic tumor microenvironment for more effective solid tumor cancer cell eradication when reintroduced into the patient.
The FDA has approved CAR-T therapies based on this technique within the last decade to treat several blood cancers. Still, CAR-T therapies can suffer from resistance over time, which may lead to disease recurrence.
Nanotein CAR-T Cell Expansion
To address this issue, Nanotein Technologies has developed a T cell activator that expands clinically potent, long-lasting T-cells. Once a patient’s isolated T cells are modified to include specialized CARs that can recognize and attack cancer cells, Nanotein’s T Cell Expansion technology activates the CAR-T cells for ex vivo expansion and generates at greater numbers of stem cell memory (TSCM) T cells.
Our NanoSpark STEM-T Soluble T Cell Activator is highly efficient, producing larger quantities of CAR-T cells in less time than our competitors and without the risk of synthetic contaminants. Contact our team for more information.
Are you looking to enhance your T-Cell activation?
Connect with Nanotein today! Get In Touch